NEWS RELEASES
FOR IMMEDIATE RELEASE
March 22, 2005
Novel ultrafast laser detects cancer at earliest possible stage
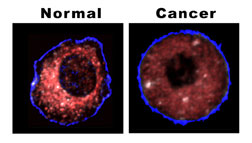 Proof positive — The difference between a
normal and cancerous liver cell is shown clearly by the
location of mitochondria, as revealed by Sandia's biocavity
laser. The healthy cell shows very few mitochondria near
the outer cell wall; they cluster densely (red coloration)
as they approach the cell's nucleous (depicted here as the
black central hole). In the cancerous cell, the mitochondria
are spread throughout the cell, do not cluster, and under
the same lighting produce a more subdued effect.
Proof positive — The difference between a
normal and cancerous liver cell is shown clearly by the
location of mitochondria, as revealed by Sandia's biocavity
laser. The healthy cell shows very few mitochondria near
the outer cell wall; they cluster densely (red coloration)
as they approach the cell's nucleous (depicted here as the
black central hole). In the cancerous cell, the mitochondria
are spread throughout the cell, do not cluster, and under
the same lighting produce a more subdued effect.Download 300dpi JPEG image, ‘— mitopic.jpg", 132K (Media are welcome to download/publish this image with related news stories.)
LOS ANGELES, Calif. — To investigate tumors, pathologists currently rely on labor-intensive microscopic examination, using century-old cell-staining methods that can take days to complete and may give false readings.
A lightning-fast laser technique, led by Sandia National Laboratories researcher Paul Gourley, has provided laboratory demonstrations of accurate, real-time, high-throughput identification of liver tumor cells at their earliest stages, and without invasive chemical reagents.
The technique generates a laser beam in single human cells pumped from a flask through tiny microchannels. The beam is altered by what it encounters. These changes, registered by an imaging spectrometer, instantly identify cancer-modified mitochondria in cells gone wrong. Mitochondria are known as the power pack of cells, energizing them like batteries do flashlight bulbs.
“There are hundreds of mitochondria, sometimes thousands, in a cell,” says Gourley. “To see them in the old way requires a time-consuming process like fluorescent tagging or a chemical reagent. We’ve found we can see them immediately by light alone.”
The techniques could be critical to advancing early detection, diagnosis, and treatment of disease.
More technically put, “To rapidly assess the health of a single mammalian cell,” says Gourley, “the key discovery was the elucidation of biophotonic differences in normal and cancer cells by using intracellular mitochondria as biomarkers for disease. This technique holds promise for detecting cancer at a very early stage and could nearly eliminate delays in diagnosis and treatment.”
The technique is effective because “it measures changes in the cell architecture, especially those arising from alterations in protein density, cytoskeleton shape, and distribution of mitochondria — changes that occur when a cell becomes cancerous,” says Gourley.
“One would think that if a cell became nonfunctional, it would become disorganized. In cancer, however, that’s not the case. A cancer cell is like an insurgent terrorist with a very well-defined agenda. It rearranges the cytoskeleton and the arrangement of mitochondria in the cell. It’s no longer a cooperative agent in a collection of cells but becomes malicious, tries to get outside the area, and hijacks the respiratory machinery of a cell.”
The biocavity laser
It is these changes — a kind of beefing-up of the
criminal forces — that Gourley’s device, called
a biocavity laser, detects.
A nano-thin layering of gallium aluminum arsenide combinations send up numerous tiny beams from a small cross-sectional generating area. These beams are reinforced or thwarted by the position and density of the mitochondria.
“The pictures we get from normal and cancer cells are very different,” says Gourley. “Mitochondria conspire to cluster around the nucleus and work together to supply energy to the healthy, functioning cell. In contrast, the mitochondria in the cancer cell sit all over, isolated and balled up in a quiescent, non-functioning state. Apparently, the rapidly growing cancer cells derive energy from an alternative source such as free glucose in the cell.”
Fortunately, the mitochondrion is nearly the same size as the light wavelength of about 800 nanometers, a frequency otherwise little absorbed by the body. Because of this close match, the laser is exquisitely sensitive to subtle changes in the mitochondria size and effects of clustering. To date, the research team has found that 90 to 95 percent of light scatter generated is from optical properties of mitochondria.
Working with UCSD
According to Bob Naviaux, professor at the School of Medicine
at the University of California at San Diego and co-director
of its Mitochondrial and Metabolic Disease Center, “What’s
attractive about this novel optical method for identifying
cancer cells is it’s a very rapid and general method
that potentially can be applied to cancer cells from solid
tumors as well as hematological malignancies like leukemia.”
Naviaux looks forward to examining a wider population of cancer cells to validate the method, combining the resources of his Center with Sandia’s laser expertise.
A project proposal has been filed with Sandia to support collaborative work between the unique research capabilities of UCSD and Sandia. “There are 300 different cell types in the human body and different mitochondria for each different shape and arrangement,” says Naviaux. “We want a library of spectra from different cell types and their cancers.”
Aiding stem cell research
Of further interest is that the biocavity laser may be applied
not only to identifying the spectra associated with cancer
cells but also those associated with stem cells, and how
these optical signals change as they differentiate into
nerve, muscle, and other tissues. “At present, there’s
no rapid method for identifying the transitional states
[of a stem cell] with the functional cell type it eventually
becomes. That process is a mysterious sequence of metabolic
and genetic changes.” There are, he says, metabolic
similarities between stem cells and cancer cells, and researchers
would like to clearly identify the differences.
“Stem cells are therapeutic,” says Naviaux. “How are their spectra distinct from cancer?”
A difficulty still ahead is viewing cancer cells in fluids taken directly from the body, rather than isolated by type in a flask. This problem will be solved by winnowing out unlikely particles through size and frequency.
Sandia is a multiprogram laboratory operated by Sandia Corporation, a Lockheed Martin company, for the U.S. Department of Energy’s National Nuclear Security Administration. Sandia has major R&D responsibilities in national security, energy and environmental technologies, and economic competitiveness.
Sandia media contact: Neal Singer, nsinger@sandia.gov, (505) 845-7078