ALBUQUERQUE, N.M. — Enabling the blind to see — a task once thought the province of miracles — is the goal of a technical team that includes Sandia National Laboratories, four other national labs, a private company, and two universities.

The idea, funded by a $9 million, three-year grant from the Department of Energy’s Office of Biological and Environmental Research, is to create 1,000 points of light through 1,000 tiny MEMs [microelectromechanical systems] electrodes. The electrodes will be positioned on the retinas of those blinded by diseases such as age-related macular degeneration and retinitis pigmentosa. These diseases damage rods and cones in the eye that normally convert light to electrical impulses, but leave intact the neural paths to the brain that transport electrical signals. Eventually the input from rods and cones ceases, but 70 to 90 percent of nerve structures set up to receive those inputs remain intact.
“The aim is to bring a blind person to the point where he or she can read, move around objects in the house, and do basic household chores,” says Sandia project leader Kurt Wessendorf. “They won’t be able to drive cars, at least in the near future, because instead of millions of pixels, they’ll see approximately a thousand. The images will come a little slowly and appear yellow. But people who are blind will see.”
The plan is to use a tiny camera and radio-frequency transmitter lodged in the frame of a patient’s glasses to transmit information and power to modules placed within the eyeball. The modules will be linked to retinal nerves that will send electrical impulses to the brain for processing.
Dean Cole, a biomedical engineer who directs the project at DOE’s Office of Biological and Environmental Research in Washington, D.C., says, “We felt that blindness is a devastating problem and that the modern conjunction of materials science with micro- and nanotechnologies in our multidisciplinary national labs offers possibilities for advances where before people had hit brick walls.”
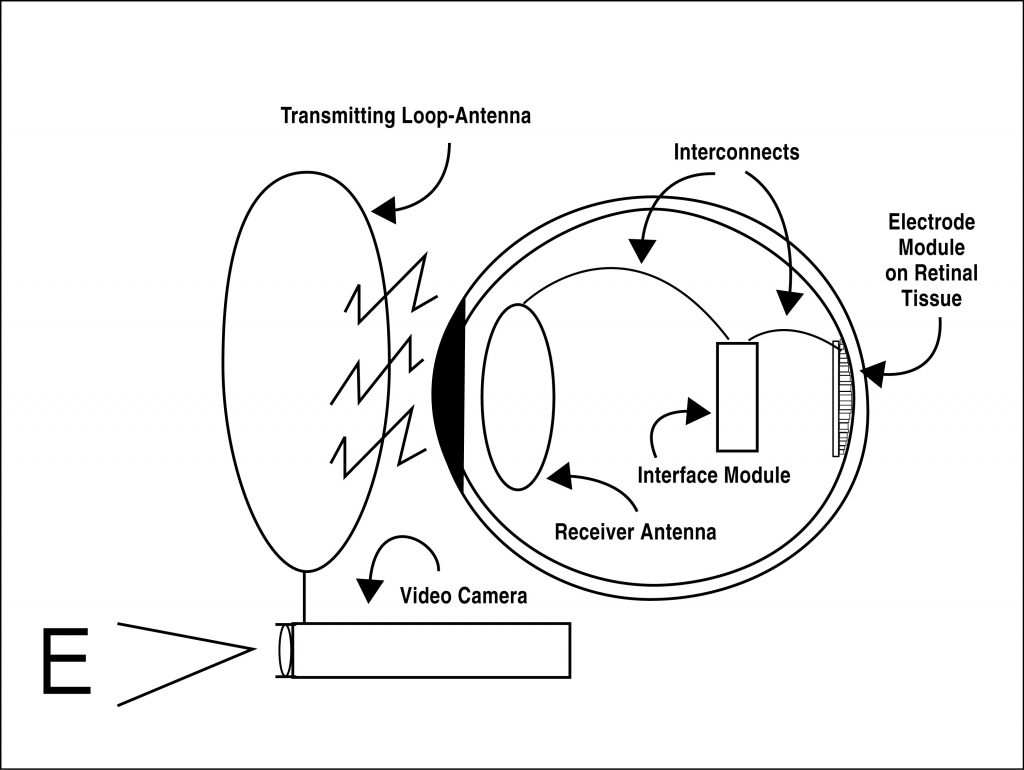
The Sandia approach is to attach a MEMs chip on the retina — that is, within the vitreous humor of the eyeball — made of LIGA and surface micromachined silicon parts. (LIGA, a German acronym for lithography, electroplating and molding, makes small parts of metal, plastic, or ceramics.) The idea is to directly stimulate some of the nerve endings within the retina to produce images good enough to read large print and to distinguish between objects in a room.
“Compared to the elegance of the original biological design, what we’re doing is extremely crude,” says Wessendorf. “We are trying to build retinal implants in the form of electrode arrays that sit on the retina and stimulate the nerves that the eye’s rods and cones formerly served.”
The size of cones and rods, as well as nerve connections, are in the micron range — a difficult but doable realm for scientists used to working with micromachines.
“We’ll use a crude, shotgun approach that fires groups of nerves. In the long run, of course, we’d like to stimulate each individual nerve,” says Sandia manager Mike Daily.
Goals of the project increase from 10-by-10 electrode arrays for fiscal year 2002 to 33-by-33 arrays for FY2004.
The project started with work at Johns Hopkins University under medical doctor and researcher Mark Humayun. When Humayun began the Intraocular Retinal Prosthesis Group at Doheny Retina Institute at the University of Southern California, the project moved with him. Teaming with Eli Greenbaum at Oak Ridge, the pair visited a number of national labs. Like Johnny Appleseeds of ideas, they tossed out seeds of thought and ultimately arranged to have each lab work on a different aspect of the electrode array/retina interface.
Said Humayun, “There is a considerable amount of advanced technology literally on the shelf or already being used for defense purposes that we could use to help solve blindness and greatly propel forward the entire field of medicine.”
Other national lab tasks include:
- The lead lab, Oak Ridge National Laboratory, will manage the multilaboratory effort as well as test the various components developed by the other labs;
- Argonne National Laboratory will investigate the viability of diamond-based electrode arrays and biocompatible coatings;
- Lawrence Livermore National Laboratory will experiment with rubberized electrode arrays; and
- Los Alamos National Laboratory will model and simulate neural paths of and from the retina to the brain.
USC personnel will implant the devices and test their medical effectiveness. Second Sight, located in Santa Clarita, Calif., will commercially produce the finished system. North Carolina State University in Raleigh leads the development of the in-situ medical electronics.
Says Daily, “Integrating microdevices into the human eye is incredibly challenging because of the need for high-reliability operation over decades in a saline environment. BioMEMs interfaces and biocompatibility issues drive much of the effort, particularly in the packaging of the microsystem.” ‘Packaging’ refers to sealing and securing a microdevice in place and linking it electronically and physically with its environment.
Counterintuitively, the rods and cones of the retina lie beneath nerves, not above them, which makes it slightly easier to connect directly to the nerves.
“The tissue housing the nerves is relatively clear. We’re investigating which electronic waveforms will best stimulate these nerves,” says Wessendorf. One problem, he says, is that “If we excite a nerve with electrons, we don’t know exactly how that compares to the electrochemical response of light on a healthy retina.”
There are other issues, he says. For one, the retina can’t handle much pressure. Thus Sandia favors spring-loaded electrodes that insure good electrode contact with minimal force. Also, protein fouling can mess up delicate interfaces intended to transmit electrical impulses. Other problems include biocompatibility — the problem of rejection of alien matter by the body — and long-term reliability.
The project, underway since October 2001, is expected to identify the most promising implantation technologies. “The question is, who’s going to engineer the best system that works in the real world?” says Daily.
Over a five-year period, says Dean Cole, the project will begin with goggles and move in the direction of corneal implants, aiming if all goes well to prepare five patients for the procedure before the project’s end. After that, he says, “The FDA will say they want 100 patients for long-term studies and DOE will get out and leave the project in the hands of industry.”
Two hundred thousand eyes in the US are blinded each year by macular degeneration, primarily in the elderly. One baby in 4,000 demonstrates retinitis pigmentosa.
Sandia is receiving $400,000 each year for its part in the research, which is led by Wessendorf and co-inventors Murat Okandan, David Stein, and Michael Rightley.
