Simulation offers hope of killing cancers without sickening patients
ALBUQUERQUE, N.M. — A patent application for a drug that could destroy the deadly childhood disease known as acute lymphoblastic leukemia — and potentially other cancers as well — has been submitted by researchers at Sandia National Laboratories, the University of Maryland and the MD Anderson Cancer Center in Houston.

“Most drugs have to go inside a cell to kill it,” said Sandia researcher Susan Rempe. “Instead, our method withholds an essential nutrient from the cell, essentially starving it until it self-destructs.”
The removed nutrient is called asparagine, which cancer cells can’t produce on their own. But there’s more to the story.
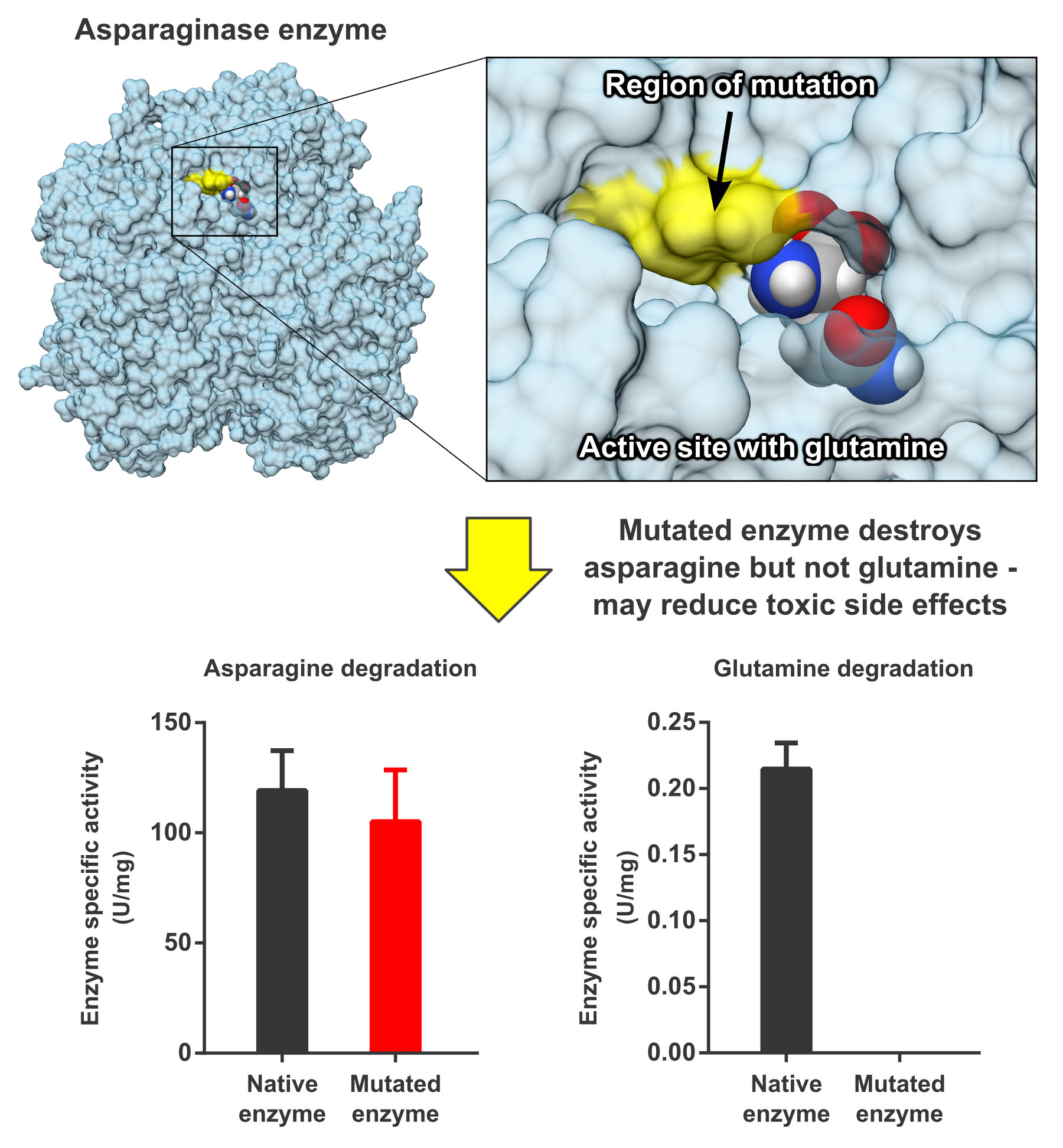
It’s well-known that chemical attempts using drugs to kill cancers often sicken the patient. In the case of the cancer drug L-asparaginase type 2 (L-ASN2), whose primary effect is depleting asparagine, side effects are generally attributed to the corresponding depletion of a chemically similar molecule called glutamine. All human cells need asparagine and glutamine to survive because each is essential to key biological processes. While most normal cells can synthesize their own asparagine, certain cancer cells cannot. So the ideal nutrient-deprivation strategy for cancers requires a difficult balancing act: Remove enough asparagine from the blood to cripple the cancer, but leave enough glutamine that the patient can tolerate chemotherapy.
The researchers at Sandia and the university did molecular computer simulations to predict what mutations would produce that desirable result when introduced into the enzyme-drug L-ASN2, commonly used to treat certain types of leukemia. The scientists’ simulations succeeded in identifying a point in that enzyme’s chain of amino acids where a mutation theoretically would eliminate the drug’s unwanted attack on glutamine.
“Technically,” said Rempe, “we simulated which parts of the two molecules came in contact with the enzyme. Then we realized that by substituting a single amino acid in the enzyme’s chain, we might avoid glutamine degradation by removing it from contact with the enzyme.”
In computer simulations, the change looked promising because the most notable difference between asparagine and glutamine was the way they interacted with that specific amino acid.
“That made us feel that a chemical change at that single location was the key,” said Rempe.
It required a mutation to change the amino acid’s chemistry. The mutation was achieved by collaborators at MD Anderson who used DNA substitutions to effect the change.
“Most researchers agree that removing glutamine from a patient’s blood was the problem in previous use of this enzyme-drug,” said Rempe. “Our simulations, as it turned out, showed how to avoid that.”
In test tube experiments, the new drug left glutamine untouched. Follow-up tests in petri dishes showed that the mutated enzyme killed a variety of cancers.
Tests underway on laboratory mice at MD Anderson should be completed by early 2016, and if they are successful, Rempe said, human testing will follow.
“If we’re wrong, and keeping glutamine intact is not the answer to the cancer problem, we’ll continue investigating because we think we’re onto something,” she said.
That’s because, she said, “we used high-resolution computational methods to redesign the cancer drug to act differently, in this case to act only on asparagine. Laboratory tests showed that the predictions worked and that the new drug kills a variety of leukemias. We hope our method can do that in a patient, and for many more cancers. But if it doesn’t, then we’ll test the opposite strategy: redesign the enzyme to destroy glutamine and keep asparagine intact. Or fine-tune the enzyme to degrade the two molecules in a chosen ratio. We’re learning to control this enzyme.”
The joint work among Sandia, the University of Maryland and MD Anderson began in 2009. Sandia managers Wahid Hermina and Steve Casalnuovo spearheaded the collaboration to use Sandia’s computational and biochemical expertise developed in national defense to help cure cancer.
Sandia’s cancer-fighting research also can be applied to building enzymes that can assist with bio defense.
Said Rempe, “If we could redesign an enzyme to break down specific small molecules, and not get diverted by interactions with non-toxic molecules, then we could apply our technique to develop safer and more effective enzymes.”
Classical modeling was performed at the University of Maryland by Andriy Anishkin and Sergei Sukharev; at Sandia, post-doctoral researcher David Rogers (now at the University of South Florida) also carried out modeling studies. Sandia post-doctoral researcher Juan Vanegas is performing quantum modeling to map out the chemical degradation process to better understand how to optimize the enzyme, said Rempe. The experiments at MD Anderson were carried out by Wai Kin Chan, Phil Lorenzi, and colleagues in John Weinstein’s group. Earlier results have been published in the journal Blood.
The work is supported by Sandia’s Laboratory Directed Research and Development office.
