LIVERMORE, Calif. — Imagine going to the hospital with one disease and coming home with something much worse, or not coming home at all.
With the emergence and spread of antibiotic-resistance pathogens, healthcare-associated infections have become a serious threat. On any given day about one in 25 hospital patients has at least one such infection and as many as one in nine die as a result, according to the Centers for Disease Control and Prevention.
Consider Klebsiella pneumoniae, not typically a ferocious pathogen, but now armed with resistance to virtually all antibiotics in current clinical use. It is the most common species of carbapenem-resistant Enterobacteriaceae (CRE) in the United States. As carbapenems are considered the antibiotic of last resort, CREs are a triple threat for their resistance to nearly all antibiotics, high mortality rates and ability to spread their resistance to other bacteria.
But there is hope. A team of Sandia National Laboratories microbiologists for the first time recently sequenced the entire genome of a Klebsiella pneumoniae strain, encoding New Delhi Metallo-beta-lactamase (NDM-1). They presented their findings in a paper published in PLOS One, “Resistance Determinants and Mobile Genetic Elements of an NDM-1 Encoding Klebsiella pneumoniae Strain.”
The Sandia team of Corey Hudson, Zach Bent, Robert Meagher and Kelly Williams is beginning to understand the bacteria’s multifaceted mechanisms for resistance. To do this, they developed several new bioinformatics tools for identifying mechanisms of genetic movement, tools that also might be effective at detecting bioengineering.
“Once we had the entire genome sequenced, it was a real eye opener to see the concentration of so many antibiotic resistant genes and so many different mechanisms for accumulating them,” explained Williams, a bioinformaticist. “Just sequencing this genome unlocked a vault of information about how genes move between bacteria and how DNA moves within the chromosome.”
Meagher first worked last year with Klebsiella pneumoniae ATCC BAA-2146 (Kpn2146), the first U.S. isolate found to encode NDM-1. Along with E.coli, it was used to test an automatic sequencing library preparation platform for the RapTOR Grand Challenge, a Sandia project that developed techniques to allow discovery of pathogens in clinical samples.
“I’ve been interested in multi-drug-resistant organisms for some time. The NDM-1 drug resistance trait is spreading rapidly worldwide, so there is a great need for diagnostic tools,” said Meagher. “This particular strain of Klebsiella pneumoniae is fascinating and terrifying because it’s resistant to practically everything. Some of that you can explain on the basis on NDM-1, but it’s also resistant to other classes of antibiotics that NDM-1 has no bearing on.”
Unlocking Klebsiella pneumoniae
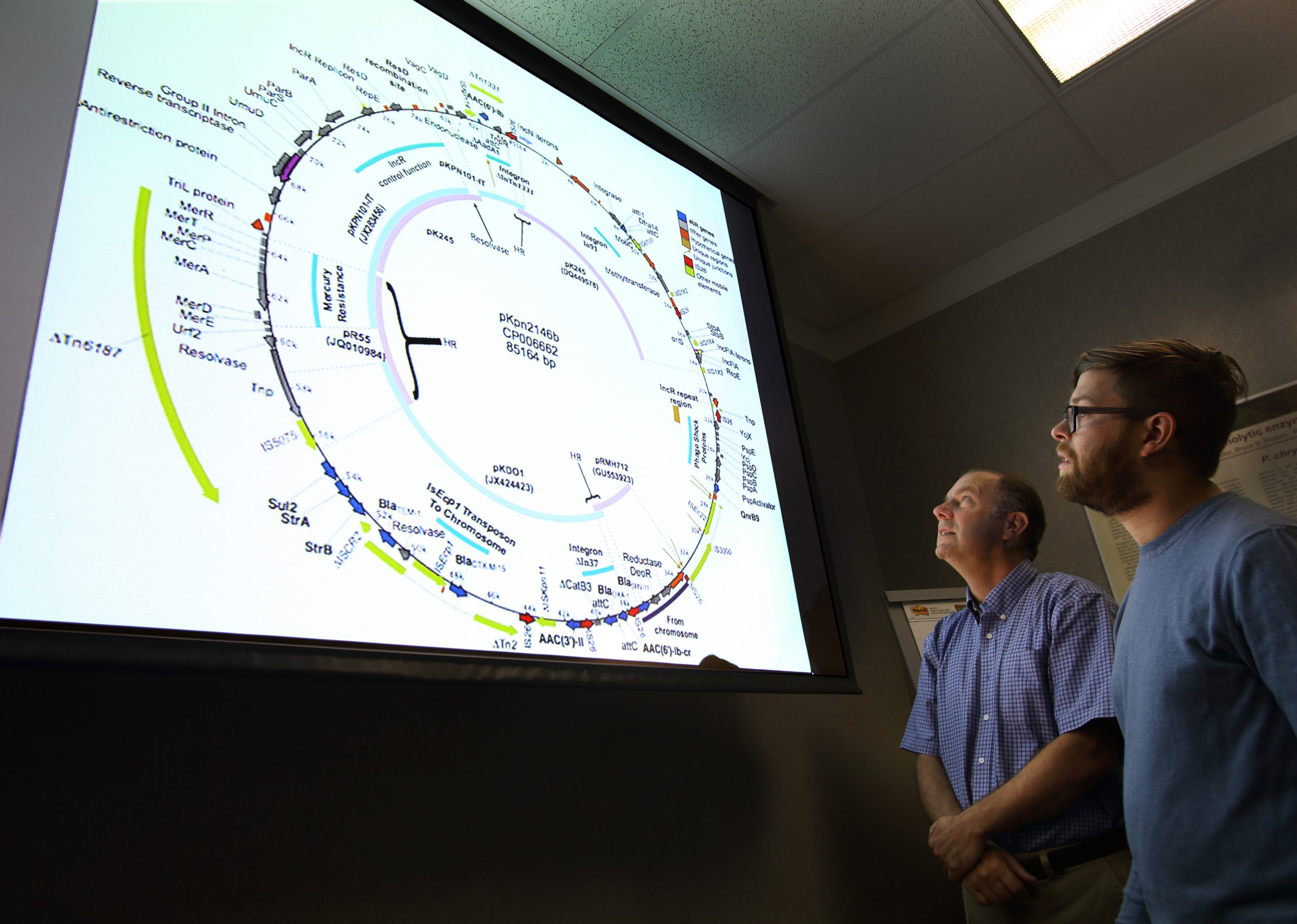
Assembling an entire genome is like putting together a puzzle. Klebsiella pneumoniae turned out to have one large chromosome and four plasmids, small DNA molecules physically separate from and able to replicate independently of the bacterial cell’s chromosomal DNA. Plasmids often carry antibiotic resistant genes and other defense mechanisms.
The researchers discovered their Klebsiella pneumoniae bacteria encoded 34 separate enzymes of antibiotic resistance, as well as efflux pumps that move compounds out of cells, and mutations in chromosomal genes that are expected to confer resistance. They also identified several mechanisms that allow cells to mobilize resistance genes, both within a single cell and between cells.
“Each one of those genes has a story: how it got into this bacteria, where it has been, and how it has evolved,” said Williams.
Necessity leads to development of new tools
Klebsiella pneumoniae uses established mechanisms to move genes, such as “jumping genes” known as transposons, and genomic islands, mobile DNA elements that enable horizontal gene transfer between organisms. However, the organism has so many tricks and weapons that the research team had to go beyond existing bioinformatics tools and develop new ways of identifying mechanisms of genetic movement.
Williams and Hudson detected circular forms of transposons in movement, which has never been shown this way, and discovered sites within the genome undergoing homologous recombination, another gene mobilization mechanism. By applying two existing bioinformatics methods for detecting genomic islands, they found a third class of islands that neither method alone could have detected.
“To some extent, every extra piece of DNA that a bacteria acquires comes at some cost, so the bacteria doesn’t usually hang onto traits it doesn’t need,” said Hudson. “The further we dug down into the genome, the more stories we found about movement within the organism and from other organisms and the history of insults, like antibiotics, that it has faced. This particular bacteria is just getting nastier over time.”
Applying findings to future work
The findings are being applied to a Laboratory Directed Research and Development project led by Sandia microbiologist Eric Carnes, who is examining alternative approaches for treating drug-resistant organisms. “Instead of traditional antibiotics, we use a sequence-based approach to silence expression of drug-resistant genes,” said Meagher.
The researchers also are applying their understanding of Klebsiella pneumoniae’s mechanisms of resistance and their new bioinformatics tools to developing diagnostic tools to detect bioengineering. Looking across 10 related but distinct strains of Klebsiella pneumoniae, they pinpointed regions that were new to their strain, and so indicate genetic movement.
“By studying the pattern of movement, we can better characterize a natural genomic island,” said Hudson. “This leads down the path of what does an unnatural island look like, which is an indication of bioengineering. We hope to apply the knowledge we gained from sequencing Klebsiella pneumoniae to developing diagnostic tools that could detect bioengineering.”
